Trichomoniasis is the most common infectious disease of the genitourinary system, which affects more than 15% of all people on earth.
Up to 180 million people become infected with the disease each year.
Consider in more detail the symptoms of trichomoniasis in women and methods of treating such an ailment.
Causes of trichomoniasis in women
The causative agent of this disease in women is the vaginal trichomonas. It affects the vagina and bladder. In most cases, Trichomonas infection occurs with unprotected sexual relations with the carrier of the infection.
It’s worth knowing that Trichomonas can survive in a humid environment up to several hours, so there are fixed cases of domestic infection with it (through washcloths, towels, underwear, etc.).
The following risk factors for contracting trichomoniasis in women are:
1. The use of other personal care products.
2. An erratic sex life and a frequent change of sexual partners (especially without the use of a condom, but even this type of contraception can not always protect against all sexually transmitted diseases).
3. The use of other people's baths, bathrooms.
4. Frequent visits to baths and saunas.
Trichomoniasis in women: symptoms and signs
After the initial infection with trichomoniasis, the so-called incubation period develops. On average, its duration is from ten to twenty days. During this time, a woman may not observe at all any manifestations of the disease, although Trichomonas bacteria will actively multiply in the body.
Symptoms of trichomoniasis in women largely depend on which particular area of the genitourinary system was affected by the disease. Most often, the patient has the following symptoms and manifestations:
1. Frequent urination.
2. Soreness during urination (burning, cutting pain).
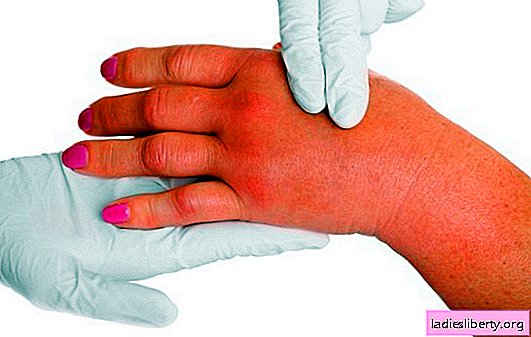
3. During a gynecological examination, swelling of the vagina is noticeable. It is also often crusty and hyperemic.
4. A sharp increase in temperature indicators.
5. Weakness and chills.
6. Headaches.
7. Drawing pain in the lumbar region.
8. Decrease in working capacity.
9. Reduced sexual desire due to pain in the genitals.
10. Quite often, itching of the genital organs is observed, which extends to the inner surface of the thighs. At the same time, sores and minor hemorrhages will occur in the comb area.
11. If the infection progresses during abortion, childbirth or during menstruation, then dangerous bacteria can penetrate the uterine cavity and cause the development of ovarian cysts or the formation of adhesions.
12. With a prolonged course of the disease in a woman, the vaginal microflora is severely disturbed. This provokes the development of vaginal dysbiosis.
Moreover, in this state, the risk of developing pathogenic flora in the vagina sharply increases (damage by yeast, staphylococci, etc.).
13. With weakened immunity, Trichomonas can affect the rectum.
If you do not start timely treatment therapy, then trichomoniasis will become chronic. In this case, the woman will suffer from inflammation for several years. In this condition, the patient can observe the following manifestations:
1. Intermittent itching and burning.
2. The appearance of foamy, mucous or purulent vaginal discharge, which can be from white to greenish.
3. Pain and discomfort during intimacy with a partner.
4. The appearance of an unpleasant odor from the vagina.
5. Dysuria.
Trichomoniasis in women: diagnosis and treatment
When the first symptoms of trichomoniasis appear, a woman needs to consult a gynecologist.
The general diagnostic scheme provides for this:
1. Gynecological examination of the patient for signs of inflammation.
2. History taking (observed symptoms). In addition, the gynecologist can ask questions about the presence of chronic diseases, bad habits, the method of contraception, the number of sexual partners, etc.
3. Carrying out PCR diagnostics.
4. Taking smears from the vagina to identify the activity of Trichomonas.
5. Taking the crop to identify the sensitivity of Trichomonas to antibiotics.
Treatment of trichomoniasis should be carried out by an experienced gynecologist. Traditional therapy is selected for each patient individually, depending on the form of the course of the disease, test results and general symptoms.
The treatment prescribes the following drugs:
1. Antibacterial drugs are used to inhibit the activity of Trichomonas reproduction. The duration of their use should be ten days. Typically, drugs such as metronidazole, clindamycin, and tinidazole are prescribed for this purpose.
2. Preparations for the restoration of microflora of women.
3. Immunomodulating drugs or adaptogens.
4. Mandatory treatment is the appointment of vitamin complexes, tinctures of aralia, aloe extract.
5. Vaginal suppositories (suppositories) with antibacterial effect (Terzhinan, Betadin, Klion) are considered very effective. Vaginal gels (Metrogil, Trichopol, Flagil) are also often practiced. The duration of treatment should be 7-10 days.
6. To destroy the enzyme component of trichomonads, preparations containing osarsol (Osarcid) are prescribed. Also with it in the complex can be used Streptocide, which has a bright anti-inflammatory effect.
As practice shows, the treatment regimen for acute and chronic trichomoniasis is practically the same. The only difference is that with a chronic lesion a woman will have to undergo several courses of therapy.
Trichomoniasis in women: treatment features, complications and prevention
During the treatment of trichomoniasis, women should adhere to such medical recommendations:
1. Treatment is desirable for both sexual partners. You cannot hide your diagnosis from a partner.
2. Sexual intercourse is prohibited during therapy.
3. A woman is recommended to exclude alcohol, have a good rest and a balanced menu to strengthen immunity.
4. It is very important to observe thorough intimate hygiene (change underwear daily, take a shower and change pads as often as possible). In this case, it is advisable to wash with special lactic acid-based intimate hygiene gels.
5. Refuse the use of sweet, fatty and fried, as such food negatively affects the general microflora (intestines and vagina). Instead, it is better to consume fermented milk products, protein foods, vegetables and fruits in large quantities.
6. Two weeks after the end of therapy, all tests should be repeated to monitor the result of treatment. If the patient is again found to have active trichomonas, then she should be prescribed stronger antibiotics to suppress the vital activity of bacteria.
If trichomoniasis is not cured on time, it can provoke the appearance of such complications in a woman’s state of health:
1. Infertility.
2. Chronic inflammatory process in the fallopian tubes.
3. Various sexual disorders (decreased sexual desire).
4. Obstruction of the fallopian tubes.
5. Cervical cancer.
If the disease occurs during pregnancy, then there is a risk of miscarriage, premature birth or fetal death.
To reduce the risk of contracting this disease, it is important for women to adhere to such medical recommendations:
1. Avoid accidental sexual intercourse.
2. Be sure to use contraception using a condom, especially with a new sexual partner.
3. Follow strict rules of intimate hygiene (do not use other people's towels, washcloths and do not give your own to anyone).
4. At least twice a year, take a control test for Trichomonas and undergo an examination by a gynecologist. The same is recommended for the sexual partner (only he should undergo examination by a urologist).
5. When observing the first signs of infection, it is important to immediately consult a doctor until the disease has become chronic.
6. When treating trichomonas in a woman, her sexual partner must also undergo examination and, if necessary, a course of therapy, otherwise the outcome of treatment for a woman may not make sense at all (infection can happen again from the carrier of the disease - men).